Breast Diagnostics
In our practice, breast diagnostics include a mammogram, ultrasound examination, breast MRI as well as a ultrasound-guided punch biopsy. In general, mammography is the standard exami-nation procedure for women over the age of 50, which can be supplemented by an ultrasound examination.
For younger women, ultrasound is usually used, while a mammography may be required. In some cases, performing an MRI may be useful for further clarification.
If lumps or structures are detected that cannot be clearly assigned, a biopsy (punch) should be performed. In our practice, we perform ultrasound-guided biopsies.
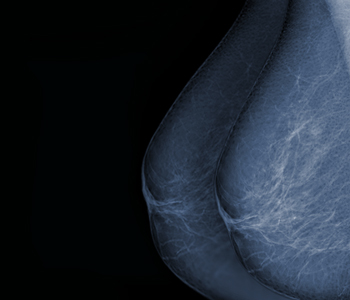
Mammography
A mammography is a radiographic representation of the female breast. We use digital full-field mammography via the Siemens “Inspiration” Mammomat, which is a state-of-the-art mammog-raphy device. The device is quality tested (constancy test) every working day. Both the medical and the assistant personnel are regularly trained and audited. Our assistants can look back on decades of experience and are here to make your examination as pleasant as possible.
When will a mammogram be performed?
- Palpable lump
- Prolonged pain
- Skin retractions or changes such as local orange skin, noticeable discolouration
- Discharge from the nipple, especially when dark in colour
- Familial burden – ovarian or breast cancer
- In case of abnormal ultrasound or MRI findings
- Inflammatory changes outside the lactation period
- Condition after breast cancer including precursors
Women between 50 and 69 years of age are entitled to a screening test as part of the German Mammography Screening, even without symptoms being present.
In individual cases, this course of action is determined by your gynaecologist.
How is a mammogram performed?
Equipment: SuperSonic Aixplorer Multiwave system with shear wave elastography and colour Doppler.
Ultrasound allows for painless and radiation-free examinations of the breast. Unfortunately, the question at hand cannot always be answered by sonography alone.
Whether a mammogram or sonography is indicated cannot be answered in general terms. Nei-ther examination replaces the other. Depending on the age, firmness and/ or size of the breast, sonography, mammography, or both may be necessary.
The fundamental advantage of a mammography lies in the excellent comparability of various images from different years and the detection of suspicious micro-calcifications.
The great advantage of ultrasonography lies in the radiation-free examination and the good dif-ferentiation between different types of tissue.
Not every cancer can be detected via ultrasonography and not every cancer can be detected via mammography depending on the examination conditions. The decision must always be made by the treating gynaecologist/ doctor in advance and on site by us.
The colour doppler can be used to visualise the blood flow of structures, which helps diagnosis in some cases.
Shear-wave elastography is a relatively new procedure in the field of breast diagnostics, which makes it possible to colour-code the strength of the tissue. Since a malignant change is usually associated with a very high consistency, this innovation helps in deciding whether cancer is pre-sent or not.
Sonography during pregnancy is not a problem either.
When will a sonography of the breast be performed?
- Palpable lump
- Prolonged pain
- Skin retractions or changes such as local orange skin, noticeable discolouration
- Discharge from the nipple, especially when dark in colour
- Familial burden (ovarian or breast cancer) in case of young patient
- In case of abnormal mammography or MRI findings
- Inflammatory changes outside the lactation period
- Condition after breast cancer including precursors
- For reasons that advocate against a mammogram
How is a sonography performed?
The patient lies on her/ his back. For better image transfer, a gel that consists of gelled water is required as a contact agent between the breast and the device. It is mild on the skin and will not stain your clothes. The images can be evaluated by the doctor straightaway. It is then decided whether further examinations, e.g. a mammogram, are required.
MR-Mammography
Equipment: Magnetom “Symphony” by Siemens with a field strength of 1.5 Tesla
Sectional images are taken by magnetic resonance tomography and are based on the deflection of hydrogen atoms in the magnetic field. The examination of the breasts requires the administra-tion of a contrast agent into the vein. The contrast agent is extremely well tolerated and allergic reactions, which we can treat immediately with medication, are very rare. At about 20 ml, the amount administered is very low. We use a high-quality product with the lowest possible risk classification. The examination is not associated with X-rays.
When is a breast MRI performed?
The statutory health insurance companies assume the costs of an MRI if,
- Neither mammography nor ultrasonography are able to determine whether there is a recurrence of cancer in the scar area following breast cancer
- A lymph node features cancer cells of which the origin is unclear
In addition, an MRI may be useful:
- in case of histologically confirmed breast cancer, to find further focal findings that cannot be displayed by means of mammography and sonography,
- for the further classification of focal findings that cannot be clearly defined via mammography and sonography,
- for high-risk patients with genetic (BRCA1/2) mutations or a severe family history of breast cancer or ovarian cancer,
- to control therapy response in neoadjuvant (preoperative) chemo- and/or radiotherapy,
- for breast implants that cannot be sufficiently examined via mammography and sonography.
How is a Mamma-MRI performed?
No special preparations are required. This examination is not possible in case of metal implants (e.g., cardiac pacemakers, drug pumps) or metallic debris (e.g., grenade fragments). The patient lies on her stomach during the examination. The breast hangs down through an indentation in the table. During the examination, a contrast agent is administered via a brachial vein. Next, the images are captured, which takes about 20 to 25 minutes and is associated with different levels of noise. It is very important that you stay completely calm and do not move. This is why you should get comfortable at the beginning of the examination. After the examination, the images are first evaluated on the device, which includes the creation of so-called subtractions. Herein, a basic image is subtracted from the images after the contrast agent was administered, which fa-cilitates and improves the recognisability of pathological findings. Thereafter, we will discuss the results with you.
Ultrasound-guided high-speed punch biopsy
If one of these examinations reveals a lesion, a focal finding, or an area that cannot clearly be classified as benign, then the next, least invasive step is a punch biopsy, a so-called “punch.” Alternatively, an open biopsy, i.e. a surgical clarification, can be performed. This, of course, involves significantly more risks (narcosis, infection, etc.) and also leads to frequent follow-up surgeries. If the preliminary examinations were not performed by us, we require the correspond-ing documents at your biopsy appointment. Please do not take any blood-thinning medications before the examination. These include aspirin (ASS), several painkillers, Marcumar, Plavix, and many others. If you have been prescribed these diluting medications by a doctor, you should consult your doctor. You should not smoke before the examination. You can and should eat and drink as normal.
After consultation, we also perform biopsies on pregnant women.
When will an ultrasound-guided high-speed punch biopsy be performed?
- In case of lumps or conspicuous areas that can be visualised by ultrasound
If the changes are only visible by other methods (such as MRI or mammography), then other biopsy types are required. Of course, we will advise you in detail.
How is a sonographically guided high-speed punch biopsy performed?
- The patient lies on her/ his back
- Depiction of the change via ultrasound and planning of access, usually from below or from the side, to protect the décolleté
- Anaesthesia of the puncture site and the access to the lump with local anaesthetic, which may initially hurt and burn for a short time
- After the onset of anaesthesia, a skin incision of about 2 to 3 mm in size is made with the scalpel, which you will not feel
- A hollow needle is positioned in front of the lump via the skin incision so that the biopsy needle can be easily inserted and removed; at least four tissue removals are required
- When taking the samples, there is a brief, slightly louder noise made by the spring of the needle (which is not painful for you and will be demonstrated to you outside of your body at the be-ginning of the examination)
- Samples are collected in a liquid-filled container and sent to a specialised lab by courier
- Removal of the needle and compression of the puncture site
- Application of the dressing
- You will stay with us for about 30 more minutes for monitoring
- The result of the biopsy is usually available the next working day
- As soon as the result is available, we will contact you to discuss the next steps
German Mammography Screening
These days, breast cancer is the most common cancer among women. Every ninth woman de-velops a carcinoma of the breast sometime during her lifetime. Although the most common, breast cancer is usually not the most dangerous type of cancer among women. As long as these conditions are recognised and treated in time, they can be cured.
Mammography screening is an early detection programme for breast cancer in asymptomatic women aged 50 to 69 years. With this examination, breast cancer can be detected early, before changes in the tissue are palpable. In addition to the increased curability, early detection also results in gentler treatment (more breast conservation, reduced lymph node removal, less chemo-therapy).
The mammography-screening programme guarantees the highest medical quality: Performed by certified professionals on tightly controlled digital equipment, our practice is one of the certified screening centres specialising in breast cancer screening. So-called recertification procedures, which are carried out at regular intervals, guarantee a consistently high standard and continuous professional development in order to provide you with the best possible treatment. This certifi-cation can only be obtained through constant fulfilment of the test criteria and proof of at least 5000 mammography images per year.
In the case of suspected breast cancer or limited access to mammography, all further examina-tions necessary will be carried out as part of the screening programme. The results and the pro-cedures dependent on those results, will be discussed jointly by the physicians involved in the screening programme.
Clip or Wire Labelling
For very small suspicious findings, we can also offer wire or clip labelling to provide localisa-tion aid to the surgeon.
How To Get Here
80331 Munich
Kontakt
Dr. med. Matthias BöheimDr. med. Andreas Vaitl
Dr. med. Johannes Vaitl
Phone 089 / 26 82 95
Fax 089 / 23 70 76 59
anmeldung@radiologie-sendlingerstrasse.de
Office Hours
Monday-Thursday8:00 - 18:00
Friday
8:00 - 14:00 Uhr

